Autoimmune Brain Panel™
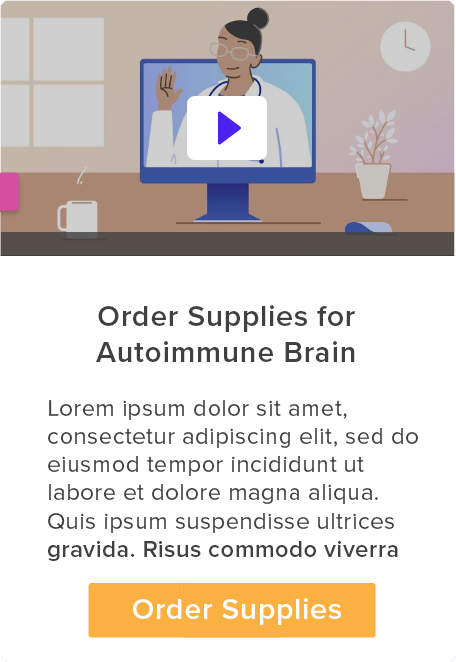
Infections ignite autoimmune attack on the brain
Sometimes, infections can confuse the immune system, triggering an abnormal immune response in which antibodies mistakenly target the basal ganglia, an area of the brain responsible for movement, mood and behavior.
This attack can disrupt how brain cells and receptors function and lead to brain inflammation (sometimes referred to as “brain on fire”), resulting in the onset of various neurologic and psychiatric symptoms.
You get an infection
The body’s immune system detects an infection (bacteria, virus, fungi, parasites) and produces antibodies to destroy the harmful organism.
Immune system attacks the brain
But the immune system goes awry and these antibodies cross the blood-brain barrier and attack an area of the brain known as the basal ganglia.

Targeting the Basal Ganglia
These “autoimmune antibodies” can bind to or block neuronal targets (Dopamine D1 and D2 receptors, Lysoganglioside GM-1, Tubulin) in the basal ganglia.
Disrupting Brain Activity
When autoimmune antibodies bind to or block these targets, they can disrupt how cells and receptors function.
Triggering Brain on Fire
This attack can lead to brain inflammation in the Basal Ganglia, a region responsible for movement, emotions and thoughts.

Leading to Neuropsychiatric Symptoms
Neuroinflammation and disruptions in how cells and receptors function in the brain can lead to a wide range of neurological and psychiatric symptoms.
Brain on Fire
How Infections and Immune Dysfunction Impact the Brain
Dr. Shimasaki discusses how common infections can trigger an abnormal immune response, leading to the onset of neurologic and psychiatric symptoms.
Common infections, like strep, influenza, mycoplasma, Epstein Barr virus, Lyme disease, SARS-CoV-2 and others, can cause the immune system to malfunction. Infectious pathogens can be bacterial, viral, parasitic or fungal.
Often times, infections are subclinical—meaning they produce no obvious physical symptoms. However, even without noticeable signs, these infections can still trigger a “brain on fire” autoimmune response.


How protected is the brain?
Crossing the blood-brain barrier.
The brain was once thought to be “immune privileged,” protected by the blood-brain barrier – a shield that prevents substances from entering the brain. However, research now shows that infections and inflammation can compromise this barrier, allowing antibodies to cross into the brain.
Once inside, these antibodies can target receptors or cells including Dopamine D1 & D2 receptors, Lysoganglioside GM1 and Tubulin ─ blocking or attaching to these targets and disrupting how they function and causing brain inflammation.
In this case review, Dr. Shimasaki examines how an underlying autoimmune dysfunction — triggered by infection — was identified as the root cause of a child’s treatment-resistant psychiatric symptoms.
Exposing Immune Triggers Behind ‘Brain on Fire’
The Autoimmune Brain Panel™ is a specialized test designed to detect infection-triggered autoimmune activity that may be affecting the brain, leading to neuropsychiatric symptoms. The test can assist clinicians in identifying whether a patient’s symptoms may be due to a treatable autoimmune dysfunction rather than a primary neurologic or psychiatric condition.
Testing is simple. And involves a single blood draw.

Take the first step towards understanding your neuropsychiatric symptoms with an exclusive guide to something here, all backed by world-leading science.


Immune-mediated neuropsychiatric disorders. We’ll review why it’s important to identify and treat these conditions and share patient success stories!
Important Information Regarding Our Emails: To make sure you don’t miss out on important updates from us, please check your spam/junk folder. If you find our email there, please mark it as “Not Spam” or “Not Junk” and add customerservice@moleculera.com to your safe sender’s list or contacts.