Could infections play a role in some cases of pediatric bipolar disorder?
Published Study: Investigating the frequency of tick-borne infections in a case series of 37 youth diagnosed with pediatric bipolar disorder
This retrospective review examined 37 youth with pediatric bipolar disorder, treated at a psychiatric practice located in New Jersey, a Lyme-endemic region. Expanding on earlier findings, the study explored whether tick-borne and related infections may contribute to the development and persistence of bipolar symptoms in children and adolescents.
Study Methods: Diagnoses were established using DSM-IV-TR and DSM-V criteria through parent and child interviews, standardized questionnaires, and school reports. Patients with pediatric bipolar disorder were screened for immune-mediated conditions such as PANS/PANDAS and tested for common infections including Lyme disease, Babesia, Bartonella, Mycoplasma pneumoniae, and Group A Streptococcus. A diagnosis required both laboratory evidence and clinical confirmation.
Hidden Infections in Pediatric Bipolar Disorder
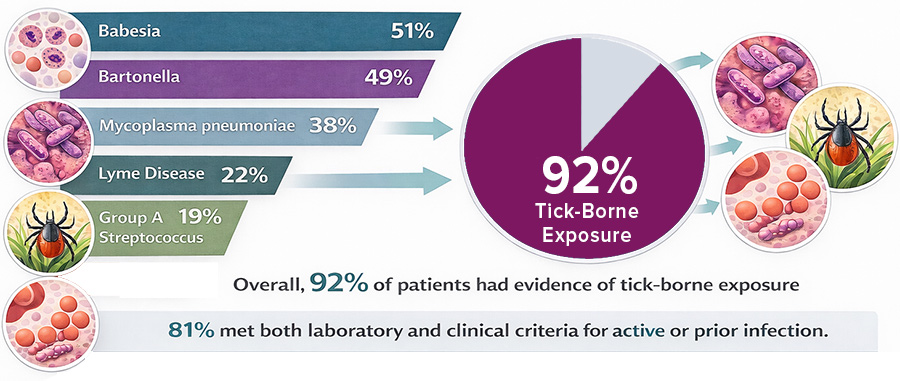
Results: Evidence of infection was common: Babesia (51%), Bartonella (49%), Mycoplasma pneumoniae (38%), Lyme disease (22%), and Group A Streptococcus (19%). Overall, 92% of patients showed evidence of tick-borne exposure, with 81% meeting both laboratory and clinical criteria for active or prior infection.
Conclusion: More than three-quarters of patients had confirmed tick-borne infections, suggesting a potential link between infection, immune dysregulation and mood instability. Given these findings, clinicians should consider tick-borne infections in youth with treatment-resistant psychiatric symptoms, particularly those consistent with pediatric bipolar disorder.
Join Dr. Craig Shimasaki for a webinar on the biology of infection-triggered autoimmune neuropsychiatric disorders and the clinical use of the Autoimmune Brain Panel™ (formerly the Cunningham Panel™) for diagnosis and treatment.
Webinar: Infection, Immunity, and the Brain: Clinical Implications for Neuropsychiatric Disease
When: Friday, February 6 at 12pm CT
Learn how the Autoimmune Brain Panel™ can help identify patients whose neuropsychiatric symptoms may stem from an infection-triggered autoimmune process.
Schedule your free, personalized 1-on-1 consultation with our Medical Relations Manager Amy Cross, NP.
RELATED STUDIES
(Bransfield R., et al. Healthcare. December 29, 2023)
A wide range of microbes—including bacteria, viruses, fungi, and parasites—have been associated with conditions such as autism spectrum disorder, schizophrenia, bipolar disorder, depression, anxiety, suicidality, and behavioral dysregulation, often through mechanisms involving neuroinflammation, immune activation, and altered gene expression.
(Breitschwerdt E., et al. Journal of Central Nervous System Disease. March 18, 2019)
An adolescent with severe, treatment-resistant psychosis for 18 months showed progressive improvement of neuropsychiatric symptoms, was able to discontinue psychiatric medications, and returned to pre-illness activities following combination antimicrobial therapy. He also experienced a resolution of Bartonella-associated skin lesions.
(Cross A., et al. Frontiers in Psychiatry. February 2, 2021)
A 7-year-old girl developed relapsing neuropsychiatric symptoms after travelling to a tick-endemic area. She tested positive for Lyme disease and multiple streptococcal infections, meeting PANDAS criteria. After 31 months of antimicrobial therapy and IVIg, she achieved complete remission and remained symptom-free at the time of publication.